
Digital Hub
Enabling cross-sector data exchange between regional healthcare facilities
Hospitals and medical practices generate millions of patient records every day, representing an enormous potential for tomorrow’s healthcare. However, the majority of patient data in healthcare organizations is still heterogeneous and unused. The Medical Informatics Initiative (MII) has already laid the groundwork for a digital infrastructure to make routine patient data usable for health research, particularly in university medicine. The data generated routinely in patient care are digitally networked and made available for medical research purposes via Data Integration Centers throughout Germany. The Data Integration Centers provide the technical and organizational prerequisites for secure and privacy-compliant access to high-quality routine health care data. At a single location, medical data is consolidated, converted into a standardized format, and made available for research and analysis projects.
In addition, the Data Integration Centers are well-connected nationwide, making it possible to carry out projects across sites. The results can be fed directly back into care, so that faster and more effective treatment and therapy options can be developed in the future.
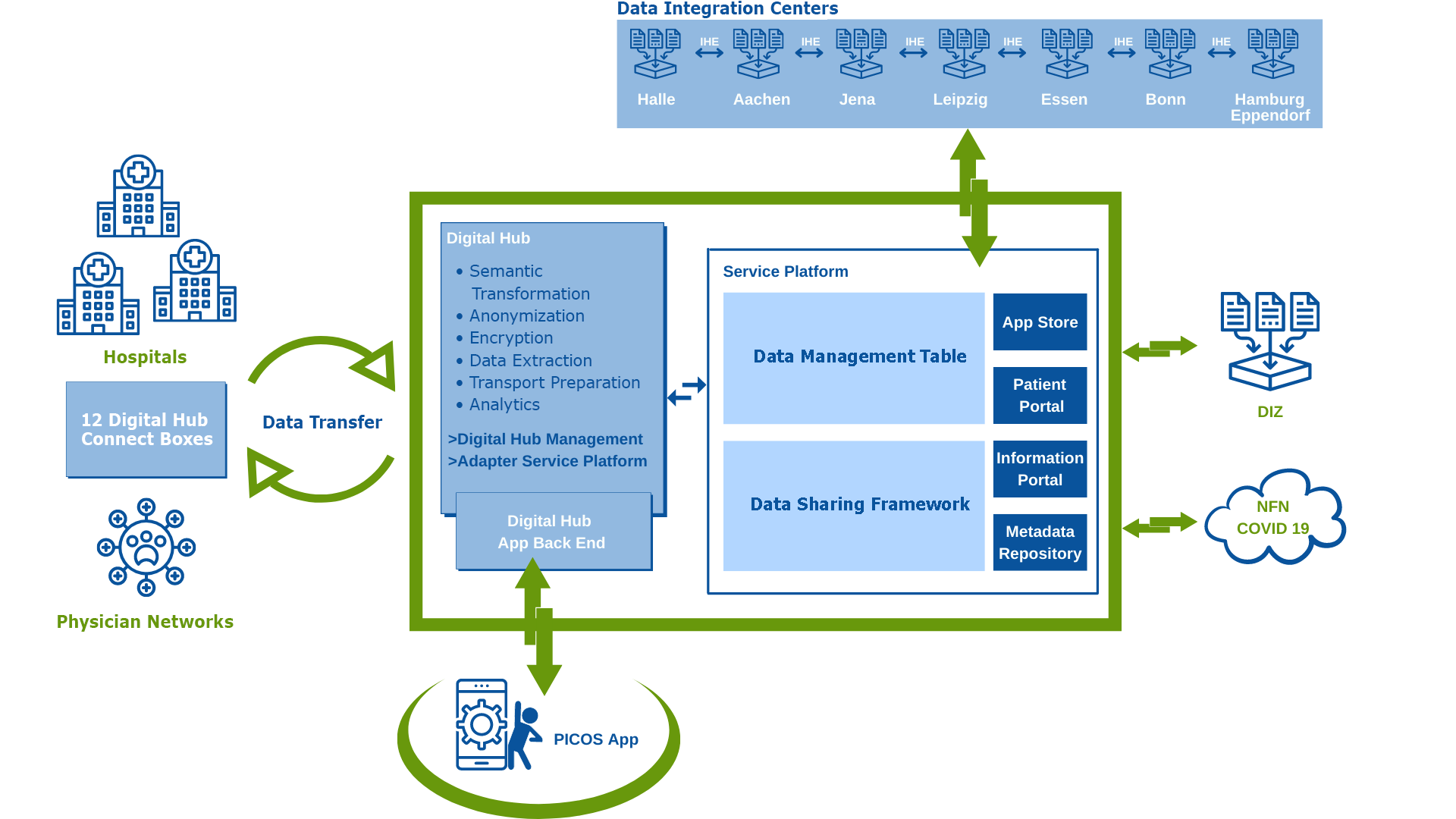
DISTANCE architecture for networking between non-university and university structures
with the Digital Hub and the existing structures of the SMITH Consortium. (Source: UK RWTH Aachen)
Improving research and care by networking regional care data
DISTANCE transfers the technical concept of the MII to regional hospitals and outpatient physician networks. The project builds on the preliminary work of the IT solutions developed in the SMITH Consortium. The goal of the project is to optimize medical care through the cross-sector exchange and integration of medical data into the MII core data set. The core data set defines the data sets, IT and terminology standards for all MII sites according to which inpatient data must be available in the Data Integration Centers. The long-term goal is to increase the availability of real-world care data, simplify access to the data, and accelerate the transfer of research results to intersectoral care.
For the first time, longitudinal data is being collected from former intensive care patients using the PICOS App. Medical data that is highly relevant for research is being collected repeatedly from the same people over a longer period of time using the app. Artificial intelligence (AI) is also used to better predict disease progression after intensive care treatment.
The heart of DISTANCE: the Digital Hub
The Digital Hub serves as the basis for cross-sector, interoperable data exchange between university institutions, participating primary and standard care hospitals, and general practitioners. The hub performs the same functions as a university hospital Data Integration Center, but is explicitly used for networking and data exchange between non-university healthcare providers. Data are collected centrally from standard care, anonymized and made available nationwide. All participating regional healthcare providers are connected via so-called Hub Connect Boxes, which are operated locally at the sites. After the end of the funding period in 2025, the Digital Hub will be continued with the help of a sustainability plan in order to connect regional healthcare providers to the MII network beyond the funding period.
The added value of the DISTANCE Hub approach is verified
Setting up and operating the infrastructure is an immense cost. Therefore, the DISTANCE project will not only assess the feasibility but also the added value of the DISTANCE Hub approach for intensive care, medical procedures and research. In order to establish MII structures across sectors in the future, it is important to estimate the costs for the roll-out partners. A long-term, nationwide roll-out will only be possible if the additional effort for this process and all operating costs can be adequately remunerated.
The ZTG Center for Telematics and Telemedicine was commissioned by the Leipzig University, as a project partner of DISTANCE, to carry out a health economic evaluation. On the one hand, this evaluation will determine the costs of DISTANCE in order to model the costs of a national roll-out of the developed infrastructure. Secondly, the costs will be compared with the expected benefits.

